Let's Talk !
Healthcare institutions and providers are transitioning from outdated paper record keeping to electronic health record technology. According to HealthIT.gov, nearly 9 in 10 (86%) office-based physicians have adopted any EHR, and nearly 4 in 5 (80%) have adopted a certified EHR. These statistics illustrate a demand for technologically advanced solutions, as it increases patient access to health information, encourages data sharing amongst providers, increases practice efficiency, the overall quality of care, and more. Though with clear benefits, many providers are still resistant. We’ve outlined common EHR implementation challenges below and ways to overcome them, in hopes of reassuring those with doubts.
Table of Contents
Electronic health records (EHRs) are real time, digital compilations of patient health data that is available instantly and are transmitted securely to authorized individuals, provided they have internet access.
Electronic Health Records (EHR) have evolved, and skilled software developers have enhanced these resources to create intuitive platforms that modernize the processes of healthcare recordkeeping and streamline patient data-sharing processes. A closer examination of EHRs' role in monitoring, collecting, and sharing data reveals payer-based, voice-enabled, and interactive two-way EHR wearables.
Amongst several challenges hindering healthcare is how insurance companies interface with healthcare providers. Several insurance companies have recently begun providing free EHR systems to better assist healthcare providers with data organization, efficient record keeping, and other critical administrative tasks required to interface with insurance companies.
Payer-based EHRs enhanced by software experts are integrated within the payer’s administrative and care management systems to allow seamless access to data and critical patient records. This system promotes efficiency and expedited access to patient data, enabling better workflow between insurance companies and healthcare providers seeking to streamline processes.
Healthcare providers have always been tasked with processing large volumes of data: patient notes, records, insurance communications, and status updates. Voice-enabled EHRs designed by adept software developers leverage modern Natural Language Processing (NLP) resources to create voice-enabled EHR platforms capable of accurately capturing voice commands. Designed to reduce repetitive tasks and expedite clinical data capture, voice-enabled EHRs are an intuitive tool for healthcare providers to reduce workloads and facilitate efficiency.
Wearable health devices continue capturing market share due to real-time data capture and optimization by software developers, and they can share data via connected devices with healthcare providers to enable customized, individualized health plans. Grandview Research reported the global wearable health device market share exceeded $26 billion in 2022 and is forecasted to grow 25% from 2023 to 2030. We see a strong demand for the versatility of EHR wearables.
Software developers can design and integrate wearable health devices that adhere to all HIPAA and HL7 standards. Creating customized, unique parameters, healthcare providers share individualized patient care plans and set data-driven benchmarks to facilitate active patient participation within care plans, creating goals of patient independence and sparking a rise in patient-reported outcomes (PRO).
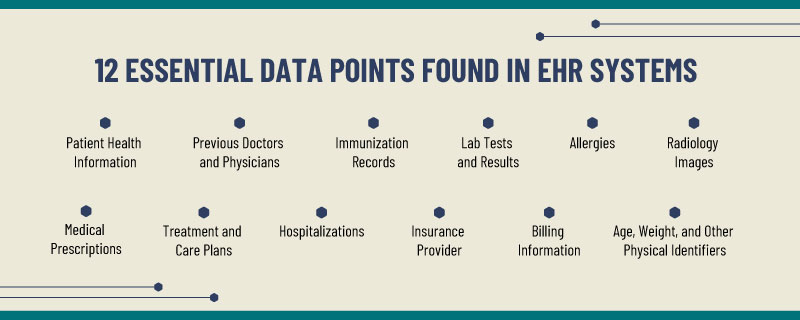
EHR systems are comprehensive and include, not only clinic data but also:
Patient medical history
Doctors seen in the past
Immunization records
Allergies
Lab test and results
Radiology images
Medical prescriptions
Hospitalizations
Insurance provider
Treatment and medication plans
Age, weight, and other physical identifiers
Integrated EHRs provide access to historical data, informing decisions made over patients and their overall care plans. According to HealthIT.gov, one of the key features of EHRs is that health information can be created and managed by authorized providers in a digital format. Integrated EHR systems are built to share information with other health care providers and organizations – such as laboratories, specialists, medical imaging facilities, pharmacies, emergency facilities, and school and workplace clinics. This capability of being shareable with other providers across more than one health care organization improves care outcomes and overall patient health.
An integrated EHR system promotes connectivity amongst all health practitioners, offices, and facilities involved in patient care. Patients also have access to this information through patient portals. These integrated systems provide instant access to patient records. You can share records with other providers, update them in real time, and ensure everyone is on the same page to provide the best care for patients. This system also automates and streamlines workflows.
If you’re still relying on paper files, here are a few reasons to make the switch to a fully digitized, integrated EHR/EMR system.
Reduces Errors and Risks: An integrated data system houses easily accessible and comprehensive medical records, speeding up diagnostics. While EHRs contain and transmit data, it also analyzes it. For instance, these systems cross check a patient’s current medication and allergies and alerts the medical team of potential conflicts. Additional benefits include, clinical alerts and reminders, enhances research and
Increases Practice Efficiency: with 30% of time dedicated to time consuming administrative tasks, EHR integrations digitize and automate these job functions. This time can then be reallocated and spent on more important tasks. For instance, these systems can be integrated with scheduling platforms to link appointments directly to progress notes, it can also automate billing, coding, and prescription refills, manage claims, etc.
Increase Patient Satisfaction: through patient portals, patients have access to all of their medical records, lab tests and results, can communicate with care team immediately, and it reduces paperwork. This accessibility to resources empowers patients to become more active in their care solutions, yielding more positive results in overall health and increased satisfaction.
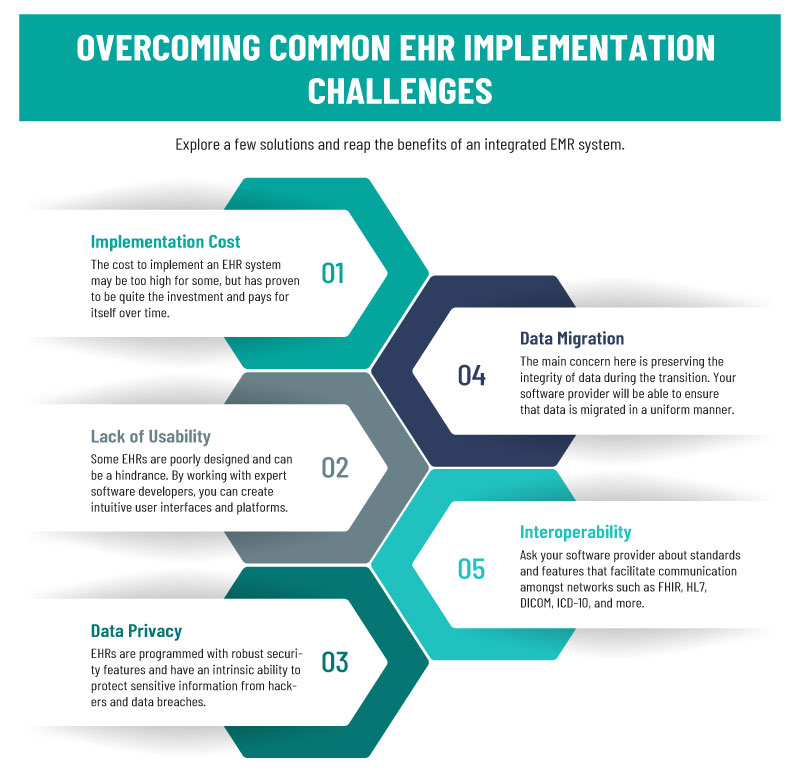
Below are the most common EHR implementation challenges we see among healthcare providers. Knowing how to address them now will save you time when integrating an EHR system.
One of the main reasons healthcare organizations resist EHR integration lies in the cost. Though it is proving to be a smart investment. A properly implemented system leads to greater revenue, reduced costs, and increased efficiency.
Some EHR and EMR systems are not functional. Rather than being intuitive and user friendly, they are poorly designed, alerts fire at inappropriate times and too often, hinders accurate data entry, they’re difficult to navigate, which can all hinder adoption in practices, clinics, etc. These issues also lead to mistakes, frustration, and can impede workflows and productivity rather than increase efficiency. Lack of usability is a serious problem. Compromised medical data can have fatal consequences.
According to David Lareau, CEO of Medicomp Systems, a provider of physician-driven point-of care solutions that fix EHRs, EHR usability can be improved by leveraging “artificial intelligence (AI)-based technologies that improve workflows and make patient and problem-specific information more accessible at the point of care.” Using AI technologies, organizations can use tools to quickly identify and interpret clinical data from multiple reference points to improve patient care and minimize frustrations and a breakdown in workflows.
Healthcare professionals may be hesitant to switch to EHR systems believing it to be counterproductive. They have to be updated every few years, updating new systems with existing patient data is an exhaustive task, and so on. However, not making the switch could prove to be an even bigger risk. Choosing to not transition to digital solutions could result in regulation violations, a decrease in revenue, increased clinical turnover, and impaired practice workflows. EHRs are programmed with robust security features and have an intrinsic ability to protect sensitive information from hackers and data breaches. They come programmed with standard security protocols, such as ONC-ATCB certifications, audit trails, protected passwords, and data encryptions.
Ask your software developer about ONC and HIPAA certifications and ensure your system is programmed with the above security protocols.
Migrating from an old system to a new one presents its own set of challenges. The main concern here is preserving the integrity of data during the transition. According to Robert Havasy, MS, managing director of the Personal Connected Health Alliance at HIMSS, “partnering with a third-party abstraction partner can help hospitals and other provider organizations more effectively plan, manage, and implement a comprehensive, long-term data integration strategy”. Teri Burley, managing senior program director at Leidos Health, also agrees that bringing in a third party could provide a solution to the data migration issue, saying, “a third-party, ideally, will have expertise in your EHR and will be able to ensure that data is migrated in a uniform manner — with the correct coding, populating the appropriate tables, and ensuring the integrity of all data integration between databases.”
Healthcare interoperability refers to the ability of several programs to share information and work together. If your EHR or EMR system cannot communicate with other systems, you lose much of the value of electronic records and data. Interoperability is essential to a functioning EHR system. The 2019 Medicare and Medicaid Promoting Interoperability Programs law created incentives for increased EHR integration. Despite passage of the law, interoperability remains an elusive goal for some EHR systems.
To address this challenge, ask your software provider about features that facilitate communication among networks. These include cloud-based systems, blockchain and application programming interfaces (API). An experienced provider will have several solutions for your EHR interoperability problems.
The healthcare industry continues to be receptive to and embracing the newest tech-driven resources designed to optimize processes. EHRs have experienced a dramatic shift from on-site solutions to more modernized, Cloud-based platforms. This shift enables the healthcare industry to reduce infrastructure expenses as third-party tech support firms monitor, update, and safeguard all crucial patient data on Cloud-based networks, shifting the costly burden of platform maintenance and updates from on-site provider personnel to software development teams, well-versed in the latest Cloud resources while offering additional cybersecurity resources dedicated to mitigating crippling cyberattacks and costly data breaches.
Artificial intelligence continues its impressive transformation of major industries, and its steady application within healthcare has created an unprecedented insight into patient success strategies and how data is valued and utilized. It continues to be an invaluable resource to create paths for modernized medicine. AI experts have successfully integrated this powerful resource within EHRs to automate documentation data collection, coupled with predictive analytics customized by software specialists; it facilitates data-driven decisions to provide personalized insight into patient care and health and even studies historical data to forecast future outcomes.
Artificial Intelligence has propelled precision medicine, a technique focusing heavily on analytics and how data is redirected to forecast future outcomes to aid in creating proactive, individualized care plans designed to thwart the onset of chronic diseases, which are largely responsible for the U.S. healthcare industry’s highest expenses.
Are you ready to experience the reduced costs, increased practice efficiency, and greater security of an EHR system? At Chetu, we have extensive knowledge and experience in Veradigm EMR and EHR integrations and develop custom, integrated systems that are interoperable, intuitively designed, easy to navigate, etc. while also meeting regulatory standards. Contact us today!
Disclaimer:
Chetu, Inc. does not affect the opinion of this article. Any mention of specific names for software, companies or individuals does not constitute an endorsement from either party unless otherwise specified. All case studies and blogs are written with the full cooperation, knowledge and participation of the individuals mentioned. This blog should not be construed as legal advice.
Chetu was incorporated in 2000 and is headquartered in Florida. We deliver World-Class Software Development Solutions serving entrepreneurs to Fortune 500 clients. Our services include process and systems design, package implementation, custom development, business intelligence and reporting, systems integration, as well as testing, maintenance and support. Chetu's expertise spans across the entire IT spectrum.
- See more at: www.chetu.com/blogs
Privacy Policy | Legal Policy | Careers | Sitemap | Referral | Contact Us
Copyright © 2000-2024 Chetu Inc. All Rights Reserved.